Hip Procedures
TOTAL HIP REPLACEMENT SURGERY
What is Arthritis?
Arthritis is a condition whereby there's damage to the joint cartilage. The most common type is osteoarthritis, which may result from previous joint injury or subtle mismatch between the ball and socket of the hip from birth. Idiopathic osteoarthritis is a term we apply to osteoarthritis of indeterminate origin. Another significant subset of arthritis arises from conditions associated with inflammation within the body. Rheumatoid arthritis is the most common of these conditions. Other causes of inflammatory arthritis include gout and systemic lupus erythematosus. Occasionally arthritis happens as a consequence of the death of the hip joint ball due to lack of blood supply; a condition referred to by the medical term Osteonecrosis.
You may be a candidate for total hip replacement surgery if you have advanced arthritis of the hip with debilitating pain, and you are not coping with activities that ordinarily form part of your daily routine. Your family doctor or other health care professional may have already suggested that you need hip replacement surgery. A brief interview followed by examination and review of your radiographs will help determine whether you are a candidate for hip replacement surgery. You will learn about the risks and benefits of the procedure, and once you are ready, surgery will be scheduled at a convenient time.
What is a Total Hip Replacement?
The hip joint is a ball and socket joint consisting of a femoral head (ball) and the acetabular cup (socket). Total hip replacement is a surgical procedure where the diseased hip joint is replaced with artificial parts.
The top section of the femur is resected. There's replacement with a metal alloy part inserted into the bone. A head made of either a metal alloy or ceramic is then attached. The socket is roughened and shaped with special instruments to accept a metal cup into which is inserted a liner made of either Polyethylene (hardened plastic) or ceramic. The head is then locked in the liner of the cup completing the procedure. The actual total hip replacement surgery takes just over an hour. Still, the entire process of administering the anaesthetic, doing the surgery and waking you up after that takes approximately two and a half hours. Please be aware that hip replacement surgery is a major surgical procedure.

Radiograph showing a replaced hip on the right and advanced osteoarthritis of the left hip
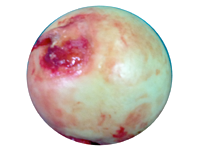
Normal femoral head - Ball part of ball and socket hip joint
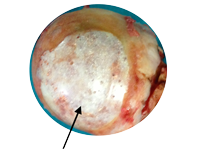
Femoral Head with severely worn cartilage
What to bring to hospital
Expect to be in the hospital for five to ten days. Please bring along a change of underwear, nightclothes and comfortable, loose-fitting day clothes like tracksuit pants, slip-on shoes and trainers (takkies). Other essential items include a small bag of toiletries and reading material.
Free WIFI is available for inpatients in the hospital, and there are personal television sets where you can access a select number of channels. Do not forget to bring along your regular walking aid and medication that you usually take.
If you use spectacles, a hearing aid or dentures, you should also bring these items with you. Please do not bring expensive jewellery and excessive amounts of cash. The hospital provides security boxes for personal belongings with only limited liability.
What to expect in the hospital
Before Surgery
The first port of call is the hospital reception. The hospital staff will be expecting you, and once formal registration has taken place, you will be escorted to the ward. Nursing staff will welcome you to the Orthopaedic department and make every effort to ensure you are comfortable. Please prepare yourself for a hospital stay for a minimum of four days. You will have blood tests, x-rays and a urine test following admission to the ward. You will then be seen by a physician who will assess the medical conditions that you have, and they may change/add medication to ensure that your state of health is optimum for total hip replacement surgery. You will be requested to sign a form that indicates that informed consent has been obtained from you for total hip replacement surgery – this is a legal requirement. The anaesthetist will visit you in the ward for a check-up and final preparation for total hip replacement surgery. They often prescribe an anxiolytic, which may leave you feeling drowsy. Some medical aid plans require that medical assessments be done on an outpatient basis before surgery. We will facilitate these consultations, and hospital admission would then be on the day of the hip surgery.
Day of Surgery
You are not permitted to eat or drink for six hours before total hip replacement surgery. Family and friends (maximum of two persons) may accompany you to theatre reception – they are not allowed in the theatre room itself. Following hip replacement, you may stay in the High Care ward for closer monitoring of vital signs. Observation is usually for less than 24 hours. A physiotherapist will visit you very early in the post-operative period to start breathing exercises, and occasionally they may get you sitting in a chair. The physician will continue to be involved in your recuperation reviewing your condition and adjusting medication as is necessary.
Day One After Surgery
The physiotherapist will do bed exercises with you, get you to stand and sit you out in a chair. If you have had an epidural catheter inserted at the time of total hip replacement surgery, your legs may still be too weak to allow you to stand. The physiotherapist decides whether it is safe to get you out of bed.
Day Two
Most of our efforts are focused on your rehabilitation from day two of your post-operative hospital stay. Physiotherapy takes centre stage and treatments will consist of a minimum of two sessions per day.
The aim is to get you standing, sitting and walking independently. The physiotherapist will supply and adjust crutches or a walker as appropriate. You need not be concerned that you will be "rushed" as the physiotherapist will supervise all treatment sessions and progress you to the next stage as you safely reach set milestones.
Day Three and Beyond
You will experience more of the same with a significant part of the day being devoted to rehabilitation treatments.
The physiotherapist will get you to negotiate stairs safely as one of the last milestones in the in-hospital rehabilitation process. Once they are satisfied that you are safe and fit to get around, they will recommend that you be discharged from the hospital. However, the final decision on discharge rests with the doctors.
Dr Mokete will inspect the surgical wound before you are discharged, and the physician also has to be satisfied that your condition is stable enough to allow discharge from the hospital.
Post-op Information/Expectations
What do I take home?
You will be discharged home with prescription medication, which includes pain medication and oral blood thinners. The pain medication will help ease any discomfort you experience. Pain occurs towards the end of the day, and the pain medication will also help you sleep better at night during the first few days at home. The blood thinners are to prevent blood clots in the legs, and these are generally taken for 28 days. You will go home with a walking aid that is appropriate for you and a toilet seat-raise if your toilet seat at home is low.
What can I expect to be able to do at home?
You will be able to walk around the house, get to the toilet without help and make yourself a sandwich and a hot beverage. Preparing a full meal will be a challenge. You should arrange for a responsible caretaker to spend the first two weeks with you to allow you to settle in at home following the total hip replacement surgery.
When do I come back for a post-operative visit?
The first post-operative visit is at two to three weeks. Please contact the office to arrange an appointment soon after you have been discharged from the hospital. During this visit, we will check with you and determine whether you are making good progress in rehabilitating the operated hip. We will also inspect the wound and advise you on appropriate wound care.
When can I expect to drive?
You can drive when you can perform an emergency stop comfortably. Driving occurs in the seventh week following the hip replacement operation. Start by driving short distances in the neighbourhood during quiet periods with little or no traffic.
When can I expect to get back to work?
In general, you can resume light duties at seven weeks if your job is mostly office-based and three months if your ordinary tasks are more strenuous. You should be in a position to put in a full day at work from four months.
Can I go to the gym?
You can go to the gym once you can confidently move about outside of the house. You should only do exercises that have been recommended by the physiotherapist and remember to take it easy in the beginning and build up slowly under the direction of the physiotherapist. Occasionally the gym may request a letter indicating that you are fit to resume gym activities – the physiotherapist will help in this regard.
What do I do with the wound?
Please do not disturb the wound dressings. We will endeavour to apply a water-resistant wound dressing which will allow you to be able to take a shower. Please do not get the operated limb into a bath. There is no need to expose the wound and to change dressings. You are likely to introduce infection from the outside by doing so. If you are concerned about the wound, please contact the office or the hospital emergency department outside office hours.
What can go wrong?
Hip replacement surgery is a significant procedure. The medical team looking after you will assess whether your body systems have the necessary reserve to withstand the operation of this magnitude.
Blood Transfusion
There is a risk of blood loss, but with modern techniques, we can get the vast majority of patients through the surgery without the need for blood transfusion.
Infection
As with any surgery, there is a risk of infection. The risk is minimal (less than one patient in a hundred) as we are meticulous with surgery and you get given antibiotics at the time of hip replacement surgery.
Blood Clots
You can develop clots in the legs (Deep Venous Thrombosis) with hip surgery, but again the risk is minimal. We administer preventative medication daily throughout your stay in hospital and extend the medication to a few weeks after your discharge. You can help reduce the risk of developing clots by enthusiastically partaking in the physiotherapy supervised exercise program before and after hip replacement surgery. Rarely the clots may migrate from the legs to the lungs compromising the function of the heart and your ability to breathe (Pulmonary Embolism).
Leg Length
The leg affected by arthritis is usually shorter than the other leg. We aim to restore the leg to its 'normal' length at the time of the hip replacement surgery, but this may not be achievable. It may not be desirable to match the length of your legs, particularly if you already have arthritis in the un-operated hip. Please take time to get used to the new hipbone. We will only consider raising the shoe to equalise the legs if you have problems after you have had the hip in place for at least six weeks.
Hip Dislocation
The ball and socket parts of the total hip replacement are maintained in place by muscle tension and orientation of the parts. There is a risk of the ball coming out of socket – dislocation. Close attention to do's and don'ts will help minimise the risk of this complication. In the rare event that the hip dislocates, please go to the hospital emergency department without delay.
Repeat Hip Surgery
Once the hip replacement parts are put into the body, they have a lifespan. The ball wears down the socket, and the pieces can become loose. Many factors determine the length of time the implants will continue to function well, but in general, the parts should last 10 to 15 years before there is a need for another hip operation.
Do's and Dont's following Total Hip Replacement Surgery include:
- Do continue your prescribed exercise routine daily.
- Do sleep with a pillow between your legs for the first six weeks.
- Do make use of aids to reach down to your toes and feet.
- Do eat a balanced diet.
- Don't squat.
- Don't sit on low chairs. You should sit in chairs with arms.
- Don't cross your legs.
- Don't reach on the outside of your feet.

